In 2005, Rand Corporation projected widespread use of electronic health records (EHRs) could save the U.S. $81 billion per year in health care. Eight years later, more than 80% of hospitals use EHRs and have received incentive payments for their “meaningful use,” yet projected savings have still not materialized. Many blamed our bloated hospitals.
We disagree. EHRs are not unsuccessful because of health care providers’ ineptness. Rather, they are a potentially disruptive technology that got caught in a legacy business model that can only prioritize sustaining innovations.
What makes an innovation “disruptive”?
Disruption does not just mean ‘idea making waves’ or ‘breakthrough technology.’ Rather, disruptive innovation theory explains how companies with cheaper, lower performing technologies target non-consumers or low-end customer segments and grow upmarket to eventually kill larger competitors with less expensive, simpler products. The personal computer, for example, disrupted the mainframe and minicomputer industry.
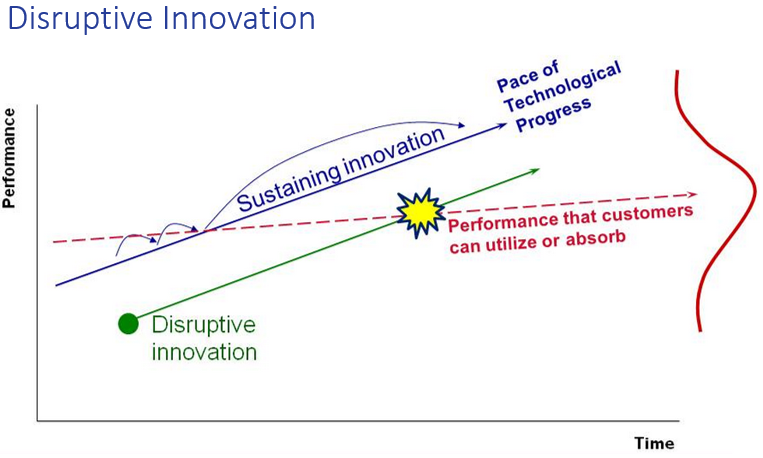
In contrast, a sustaining innovation targets demanding, high-end customers with better performing, more complex products. Next year’s car model is a sustaining innovation. It’s sleek, has more horsepower than most of us could ever use, and costs more than last year’s model. Sustaining innovations result in wonderful, high performing products but not lower prices.
The reason EHRs are not “roiling the healthcare landscape” with disruption is not that the technology is bad—rather it’s the business model in which they are being implemented. While there is some evidence that EHRs can help to increase healthcare quality, the technology is by and large being crammed into sustaining business models and used as an expensive sustaining innovation to replace paper records with complex electronic systems. Implementing new technology to sustain the way you already make money almost always keeps costs high and prevents true disruption. Indeed, the history of innovation is littered with companies that had a potentially disruptive technology such as EHRs within their grasp but failed to commercialize it successfully because they did not couple it with a disruptive business model.
Business model lock-in
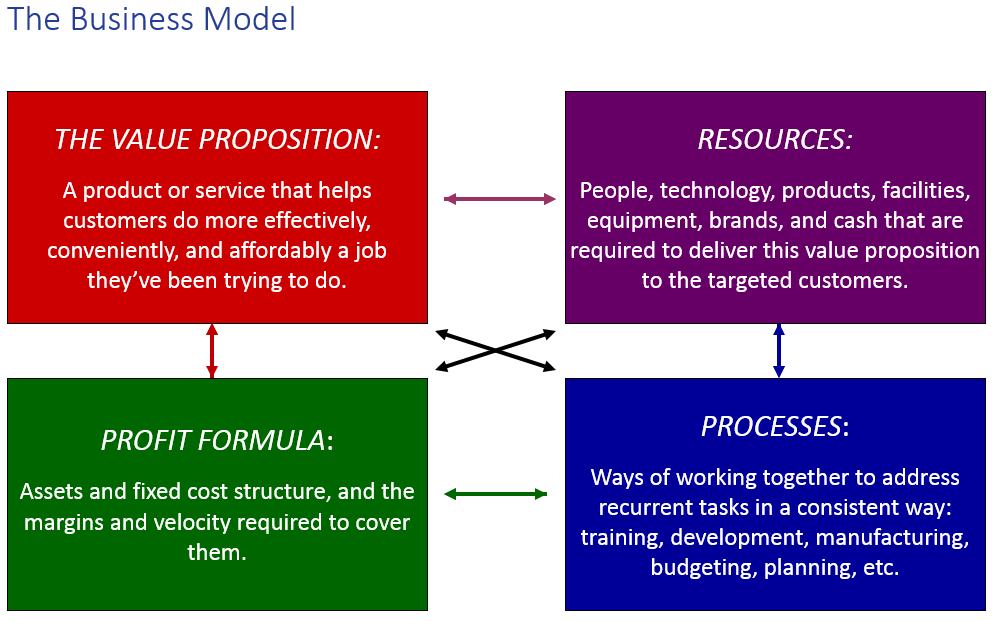
All business models begin with a value proposition, then combine resources and processes to deliver that value proposition profitably. Once profitability comes the company “locks” its business model. Business model lock-in often prevents companies from disrupting themselves because they try to use potentially disruptive technologies in sustaining ways, fitting them into their already-existing processes using their previously-arrayed resources to sustain existing profits and costs.
Nypro, a plastic molding manufacturer, saw this play out in the mid-1990s. Nypro’s value proposition centered on producing precision parts in high volumes. The CEO saw that high-volume demand was beginning to be replaced by demand for a wider variety of parts with low volume production runs. To address this emerging need, Nypro’s engineers developed a new molding machine, the Novaplast. In order to leverage existing assets, the CEO offered to lease the machine on attractive terms to his each of his plant managers.
Only nine plant managers took him up on the offer, and seven of them returned the machines after just three months.
Why did the machines fail? It wasn’t that the technology was crummy. Rather, salespeople had little reason to call on or prioritize low-volume customers when all the incentives of the sales process were aligned with turning out high-volume runs for their existing customers. Their potentially disruptive Novaplast technology got caught in a sustaining business model that was locked. Thus, the Novoplast had very little impact within the company. No one was at fault; it’s just the way that their manufacturing business model aligned.
Failure of “plug and play” EHRs
EHRs are following the same trajectory as the Novaplast machine. Health leaders see their disruptive potential. Yet most record systems are implemented as sustaining “plug and play” replacements for paper records, just as the Novaplast was implemented as a direct replacement for Nypro’s other molding machines. Clinicians using EHRs have little reason to use the new electronic system differently from the old paper system, and so EHRs often neither decrease cost nor increase quality. They’re just next year’s more expensive model of paper-based patient records.
No one is at fault; it’s just the way that the hospital business model aligns.
Recommendations
Fortunately, there are ways to avoid the trap of the sustaining business model and reap the benefits of harnessing EHRs as disruptive innovation. We offer two simple recommendations.
- EHR designers should create the systems based on the doctor’s job to be done. Many EHR systems attempt to duplicate paper records, but for many doctors, paper records still cost less and are much more convenient than electronic versions. EHRs often do not conveniently provide the necessary patient information at every point in the care process. EHR designers need to think beyond fulfilling legal requirements and providing the same capabilities of a paper system to providing new and better organization, analysis, and information accessibility benefits that fit doctors’ true needs.
- EHR users must think beyond merely replacing their old record systems. By investing substantial amounts of financial and human capital in systems that do little more than replace paper records and bring in incentive money from the government, health care providers are setting themselves up for eventual failure. They will never see the promised benefits because the surrounding business model has not changed. Instead, EHR-using practices need to create teams with the authority to implement systems that use EHRs to replace not just paper-based record systems but also patient check-in, insurance processing, and all other information-limited processes. Companies such as Phreesea demonstrate how electronic records in disruptive business models could make many health care jobs simpler, lower cost, and higher quality. CVS MinuteClinic uses electronic records to not just record data, but also to guide practitioners through exams and automate peer-to-peer chart review. Facilitated networks could utilize EHRs based around patient's needs. This type of innovation completely re-imagines the health care business model in a way that enables EHRs to keep their cost-cutting, effectiveness-increasing promises.
1. One of the facets of the Accountable Care Act (ObamaCare), is the development of Accountable Carr Organizations (ACOs). These are large collections of health care services meant to save costs by “coordinating care” and this recieve incentive payments via “shared savings.” Pilot data is mixed about success, but the result is the expansion and conglomeration of large health care institutions. The result of this is the buying up of thousands of small independent medical practices to become employed physicians. Those small independent practices that were previously using small (potentially) disruptive EHR providers (see DrChrono or Practice Fusion) are now forced to abandon those systems to use the hospital/health care system’s Enterprise class EHR such as Epic or Cerner. These large EHR systems are increadibly expensive, hostile to end users needs, and have no ability to coordinate care or save costs. This type of consolidation will destroy small startups and entrench established players like Epic.
2. The Job to be done for the current crop of EHRs is not to improve care or user experience. The job to be done is to maximize revenue collected by catering to an archaic payment system of fee for service and E&M/CPT coding, hijacked by the draconian American Medical Association. Do more, document more, code more, and bill more are the incentives in this current payment system in US healthcare. Quality of care payments are talked about, but very hard to implement. Without a change to the billing and payment structure, the documentation and coding burden still exists, and the EHR will never advance beyond the paper chart.
by Ben Wanamaker and Devin Bean August 8, 2013
Additional Comments
The one area in which EHR disruption can flourish would be in Direct Care practices (see Atlas MD), as third party insurance is not accepted, eliminating the need for huge chunks of mundane documentation and opening the door for new interaction models ( texting, web visits, telegraph, data portability, etc.
The history of innovation is littered with companies that had a potentially disruptive technology such as EHRs within their grasp but failed to commercialize it successfully because they did not couple it with a disruptive business model.”
This federal government (and its federal advisory committees) controls both the HITECH program (the part of the stimulus that provides incentives for adoption and “meaningful use” of certified EHRs) and the roughly half of healthcare spending in this country.
From the start, the timing, structure and incentives for the HITECH program have been misaligned with the new coordinated, patient-centered and accountable care models encouraged by health reform. In other words, the functions required of EHR vendors to be certified, the actions that providers need to take to receive EHR incentive payments and the success metrics of the program (i.e. adoption) are different than those required to support these new models of care.
EHR technology might not all be “bad” but much of it is not good. HITECH drove the rapid adoption of whatever was on the market: primarily the same warmed-over ’90′s technology that very few providers would invest their own money in prior to the program. The program focused EHR vendor resources on adding new, HITECH-specific functions to legacy platforms, often of functions desired by actual customers. And usability and quality of development is spotty at best with a recent survey finding that “92% of practices currently describe their current EHR as “clunky” and/or “difficult to use.” (http://www.prweb.com/releases/2013/7/prweb10926499.htm). Reduced fee-for-service productivity is an expectation and we might as well be in 1992 with regard to interoperability and data exchange between systems.
On the contrary the recommendation that EHR designers create systems based on the job to be done is a few years too late. Especially in health systems, yesterday’s systems have all been bought and the money has all been spent. Switching costs are extremely high and hospital administrators are loathe to risk purchasing systems from new market entrants. Perhaps the taxpayers and Congress will be happy to drop another couple dozen billion dollars to buy better EHR systems in the future, but in the meantime I fear that what we have is what we’re going to have, incremental improvements and lipstick-on-a-pig usability improvements aside.
It is the business model of healthcare that limits the development and implementation of innovative technologies. However I would counter that if a EHR were developed that actually mimicked a paper chart it would be widely adopted. Clinicians like paper because it is: easy to use, accessible, mobile, task-based, workflow-based, and logically organized. You can hardly say the same for most enterprise-wide EHR systems.
EHR designs can trace their lineage not from paper T-Sheets, but from billing systems, so they can ultimately support billing. HITECH and ACO’s only reinforce these systems because the business model has not changed. To the point of the authors, the ACO is sustaining innovation on the same business model of healthcare that has existed since WWII.
The one great change to the current business model of healthcare that would open up the truly “meaningful use” of technology would be the elimination of employer based health insurance. This would immediately shift the focus to the person as an individual, incentivize the user of PHR’s, force interoperability standards on vendors (similar to an ATM card working at any bank), and open the gates to real innovation in healthcare because the business model would be turned on its head the the technology would follow.
More issues:
1. The primary purpose of clinical records is communication among caregivers from past to present and present to future in order to avoid errors caused by human memory failure. Everything else is important and useful, but secondary to clinical communication over time.
2. To communicate, paper records weren’t the best choice. They were the only choice. Thus, paper records should not be used as the model for EHR. However, they are what we all learned, use and know. That cannot be ignored.
3. Psychology has shown the advantages and limitations of human attention and memory. EHR must be designed around those perceptual and cognitive factors.
4. The underlying healthcare “business model” problem is that providers own the patient’s record. And there are hundreds of thousands of individual provider – not patient – records.
Disruptive innovation is hard when conformity is legislated or worse lobbied into legislation by highly educated, very corrupt people with lot to gain from the faulty US system of reimbursement. EMRS have failed to serve their intended purpose- PAYMENT DENIAL MANAGEMENT. The biggest beast in the room is the third party administration of payments that shields the consumer( patient) and the medical-industrial complex from negotiating rates directly and paying fair value for services.Without tackling this fundamental problem we can see no meaningful process improvement. The only process improvement we will see is changes to maximize collections.
Why should an employer bear any part of an employee’s cost of healthcare? If they still want to do it, don’t pass that charge to taxpayers( reduced taxation for employer). Why is it a significant part of medical establishment ( I would say upwards of 70%) is geared toward billing and collection and not taking care of sick people? Why do we have the ostensible” NOT FOR PROFIT” moniker for hospitals that are sapping up taxpayer money and wasting them on useless things like bad EMRs, bloated administrative staff,making RNs into clipboard staff to unleash these horrors on other employees who just want to do their work and go home?
CMS may have belatedly realized the follies of paying AMA for CPT codes. This upcoming rule ( http://www.hcpro.com/HIM-295281-859/Tip-CMS-proposal-could-change-EM-dramatically.html ) may end the rush of hospitals taking over physician practices. A sort of creative disruption but delivered with a machete. It will also kill a lot of decent physicians, a profession now hard to train properly ( because the most seasoned teachers and practitioners have walked out of the profession already) . The really ill people need real doctors.
As a stand alone solution, replacing paper is not enough of a value proposition. The value is created when an EHR actually supports a better business outcome, which can occur in multiple ways. Patient portals, and patient access to their own medical records will be integral for a medical practice to survive and compete in the future. Excellent patient communication will also be critical. In addtion, facilitating well organized patient records, with the ability to sort a patient record in multiple ways adds value to patient care as well. E-prescribing, secure doctor to doctor messaging and remote access to patient records can add substantial value to the patient care proposition. Unfortunately, the EHR world is filled with false promises and marketing noise. We have an EHR solution that not only mimics patient charting, is completely flexible and “low-tech”, but also provides all of the unique features that can truly improve revenue, profitability, patient care and efficiency.
No comments:
Post a Comment